Sexual Health Needs Assessment
This Needs Assessment describes the sexual health needs of residents of the London borough of Wandsworth. It draws on evidence gathered through epidemiological analysis and has informed the development of the Sexual Health Strategy with a focus on prevention.
This document is also available in PDF format: LBW Sexual Health Needs Assessment 2018
1. Executive Summary
Unplanned Pregnancy
- Teenage Conception rate similar to England and London, following a substantial decline in the last decade.
- Over two thirds (70.1%) of women use user dependent methods of contraception (UDM), this is higher than England (62%). Lower percentage of women using LARC compared to England.
- All age abortions rate similar to England.
Sexually Transmitted Infections
- STI diagnosis is higher than England and London.
- STI rate is twice that of England.
- Gonorrhoea rate is three times the England rate.
- Syphilis rate 4 times that of England – mainly in men who sex with men and associated with risky behaviour.
- Genital herpes rate twice that of England.
- Genital warts rate was highest in England in 2016.
- Young people, LGBTQI and Black people experience a disproportionately high rate STIs.
- New STI rate of diagnosis in young people twice that of England.
- High rate of chlamydia diagnosis in young people.
- 40.5% of those tested had Chlamydia.
- 12% of 15-year-olds in Wandsworth partake in 3 or more risky behaviours (including smoking, drinking, and cannabis, use of other drugs, poor diet and low physical activity).
HIV
- High prevalence area for HIV and new diagnosis rate is double that of England.
- Estimates suggest approximately 181 people are unware they have HIV.
- Between 2014 and 2016, almost a third (32%) of people diagnosed with HIV were diagnosed late.
Deprivation
- The most deprived population experience the poorest sexual health, with a clear gradient in Wandsworth in STI rates between the most and least deprived areas.
2. Introduction
Improving sexual health is a public health priority. Sexual health affects the population across the life course. Poor sexual health can have not only physical but mental health implications. Sexually transmitted infections (STIs) and unintended pregnancies can have long-lasting and costly impacts on both individuals and wider society. However, they can be reduced through safer sex practices such as the use of condoms and regular testing. Sexual health services currently focus on treatment for sexual health transmitted infections, HIV and unplanned pregnancies as well as prevention. Evidence shows that a focus on prevention can improve sexual health and deliver savings to sexual health commissioners and the wider system.
2.1. Aim
This Needs Assessment report sets out the current and future challenges that maintaining good sexual health presents to people, their carers, friends and families, the local authority and the NHS in Wandsworth.
It seeks to identify key messages to guide the development of good quality, accessible sexual health services with an increased focus on prevention for the population of Wandsworth.
2.2 Audience
This Needs Assessment report is intended to inform the policies, strategies, development and commissioning plans, and practice in local organisations including Council teams, NHS organisations such as the Clinical Commissioning Group (CCG) and Trusts, and other organisations, such as the voluntary sector and representatives of the public and patients.
3. Background
The resident population in Wandsworth is 314, 544. The health of the opulaiton is mixed. Life expectancy at 65 years old is significantly worse than the London average for both men and women. There is significant variation within the borough; life expectancy is 9.3 years lower for men and 4.5 years lower for women in the most deprived areas of Wandsworth than in the least deprived areas (JSNA, 2018).
Sexual health is defined by WHO as “a state of physical, mental and social well-being in relation to sexuality. It requires a positive and respectful approach to sexuality and sexual relationships, as well as the possibility of having pleasurable and safe sexual experiences, free of coercion, discrimination and violence.”
Sexual health is a whole population and life course issue; in early childhood children begin developing their sense of identity and relationships with those around them, during adolescent young people begin to develop their independence and form sexual health relationships. By adulthood most of the population are sexually active and require support, such as good contraceptive services, information and treatment services, to maintain good sexual health.
Poor sexual health can result in substantial costs to individual and society across health, housing, education and social care. Economic modelling estimates that the wider publicsector costs of unintended pregnancy and STIs will be £27–57bn cumulatively between 2015 and 2020 (FPA, 2015). However, this modelling was based on 2015 levels of access to contraceptive and STI services (ibid.). But the substantial reduction in teenage conceptions under the former national Teenage Pregnancy Strategy (1999) was delivered using a prevention framework, which provides strong evidence that a preventive approach can redress this.
PHE and partners have published several documents to support sexual health commissioning and prevention:
- A Framework for Sexual Health Improvement (2013)
- Making it work: a guide to whole system commissioning for sexual health, reproductive health and HIV (2015).
- Good progress but more to do: teenage pregnancy and young parents (2016).
- Improving the health and wellbeing of lesbian and bisexual women and other women who have sex with women (2018)
There are 3 sexual health indicators in the Public Health Outcomes Framework:
- Chlamydia detection rate (15 to 24-year olds)
- people presenting with HIV at a late stage of infection
- under 18 conceptions
The previous needs assessment was undertaken in 2015 using data relating to 2013, and where possible the current data (2016) is compared to it. Overall sexual health is worse than the England average.
4. Local Picture
4.1 Unplanned Pregnancies
4.1.1 Teenage Conceptions
Teenage parents and their children experience poorer health, educational and economic outcomes and inequality (PHE, 2018). There is a strong relationship between teenage conceptions and deprivation. Wandsworth has an average level of deprivation compared to other local authority areas in England (deprivation decile 6) but has significant pockets of deprivation.
In 2016, there were 77 conceptions in under 18 women, which is a rate of 20 per 1000 population and lower than the England (18.8) and London (17.1) rate. This is a decrease from 2012 when there 85 conceptions in women under 18 and the rate was 25.4 in Wandsworth. Over the last twenty years there has been a substantial decline in teenage conceptions from 77 conceptions per 1,000 in 1998.
4.1.2 Abortions
Termination of pregnancy (abortion) rates are used as a proxy measure for unplanned pregnancies. These pregnancies result from the absence of, incorrect and inconsistent use of contraception.
In 2016, 23.4% of total conceptions (approximately 1,433/6125) in Wandsworth ended in abortion which is similar to England (21.8%) and London (25.4%). Over three-quarters of abortions occurred in over 20s. The largest number of abortions occurred in the 25-29 age group (397), which is over nine times the under 18 age group (46) and four times the 18-19 age group (67) (ONS, 2018).
In 2016, 38% of all abortions were repeat abortions, which consists of 40% repeat abortions in over 25s and 34% in under 25 (ONS, 2018). The percentage of repeat abortions in Wandsworth is similar to London (41.9%) and England (38.4%) (ONS, 2018).
However, the percentage of teenage conceptions ending in abortion, is significantly higher than England (58.4% compared with 51.8%) but lower than London (63.7%).
4.1.3 Contraception
The main cause of unintended pregnancies is incorrect and inconsistent use of contraception.
User dependent methods (UDM) were the most popular form of contraception used by residents with 70.1% of residents using UDMs such as the oral contraceptive pill and barrier methods like condoms, which is higher than England (62.1%). In 2016, 24.3% used LARC (excluding injections) and 5.6% injectable contraception compared to 28.1% LARC (excluding injections) and 9.8% injectable contraception for residents in England.
Long Acting Reversible Contraception (LARC) is the most effective form of contraception. LARC usage is significantly lower than England in 2016 with total prescribed LARC, excluding injections, with 36.8 per 1,000 compared to 46.4. But it is similar to London (36.8). Injectable contraception is excluded from the LARC category due to reliance on users’ compliance to turn up promptly for subsequent dose every 12 weeks. In addition, emergency contraception is excluded from the LARC and UDM totals.
The majority of LARC was prescribed in primary care at 22.7 per 1,000, which is lower than England at 28.8. The rate prescribed in the other settings was 14.1 per 1,000 compared to 17.6 in England. In 2016, Wandsworth was ranked 233 out of 326 local authorities in England for the rate of GP prescribed LARCs (1 is the highest rate), with a rate of 22.7 per 1,000 women aged 15 to 44 years, compared to 13.9 in London and 28.8 in England (PHE, 2017). However, the data do not include LARCs that have been prescribed in other services, such as termination of pregnancy (TOP) services, which may be a significant amount (PHE, 2017).
4.2 STI Diagnosis
In 2016, 5,595 new sexually transmitted infections (STIs) were diagnosed in residents of Wandsworth, 1,778.8 per 100,000 residents. This is significantly higher, and more than double, the England rate of 750 per 100,000.
4.2.1 Reinfection Rates
Reinfection rates are a marker of persistent risky sexual behaviour; between 2012 and 2016 an estimated 7.5% of women and 12.2% of men presenting with a new STI became reinfected with a new STI within 12 months. This is similar than England with an estimated 7.0% of women and 9.4% of men presenting with a new STI became re-infected within 12 months (PHE, 2017).
In Wandsworth, an estimated 6.4% of women and 15.2% of men diagnosed with gonorrhoea at a SHS between 2012 and 2016 became re-infected with gonorrhoea within 12 months. This is significantly higher than England with an estimated 3.9% of women and 10.7% of men becoming re-infected with gonorrhoea within 12 months (PHE, 2017).
4.2.2 Chlamydia
Chlamydia is one of the most common sexually transmitted infections and is frequently asymptomatic. However, untreated Chlamydia can lead to complications such as long-term pelvic pain, pelvic inflammatory disease, ectopic pregnancy and infertility in women. Sexually active young people are at highest risk. The National Chlamydia Screening Programme (NCSP) aims to control chlamydia through early detection and treatment of asymptomatic infection, so reducing onward transmission and the consequences of untreated infection. The programme screens young people aged 15-24 years old and treats those with detected Chlamydia and their partners.
In 2016 the chlamydia detection rate per 100,000 young people aged 15-24 years was 3,057 (compared to 1,882 per 100,000 in England) in 2016. 12,582 tests were carried out with 949 positives, which represents 40.5% of those tested. The Chlamydia detection rate per 100,000 young people aged 15-24 years was 3,057.3 (compared to 1,882 per 100,000 in England) in 2016; Wandsworth is ranked 6th out of 33 for London (with 1 being the highestrate) and 14th out of 326 local authorities in England (PHE, 2017).
4.2.3 Gonorrhoea
Untreated Gonorrhoea can lead to complications such as long-term pelvic pain, pelvic inflammatory disease, ectopic pregnancy, and infertility in women. Prevalence is highest amongst young adults, black Caribbean people and men who have sex with men (MSM). (Surveillance of Antimicrobial Resistance, 2017)
In 2016, the rate of gonorrhoea diagnoses per 100,000 was 219.6 (compared to 64.8 per 100,000 in England). This is the 13th highest rate of infection amongst English local authorities. The rate and number of gonorrhoea diagnoses are lower than 2013 with 772 diagnoses (246.6 per 100,000) compared with 706 diagnoses. However, combined the trend between 2014-2016 is an increase as numbers and rates rose in 2014 and 2015.
4.2.3.1 Gonococcal Resistance.
In 2016 the first documented global case of treatment failure (antibiotic resistance) was detected in the UK. Cases have occurred in both MSM and heterosexuals, and have been reported from across England, although more than 50% of cases were from London in 2017. As of June 2017, nationally there were a total of 81 confirmed cases. (PHE, 2017)
4.2.4 Syphilis
Syphilis is caused by bacteria and, if left untreated, it can have very serious complications. However, it is easily treated.
Most syphilis diagnosis are in men, especially MSM, and high rates of syphilis are associated with risky behaviour (PHE, 2017). Men who are infected with syphilis have an increased likelihood of developing HIV in the future. In 2016 46.4 per 100,000 residents were diagnosed with syphilis, which is significantly higher than England (10.6) and is part of trend of getting worse since 2012.
4.2.5 Genital Herpes
Herpes is a long-term condition caused by the herpes simplex virus. There is no treatment for herpes but medications can reduce the duration and frequency of herpes outbreaks.
In 2016, the rate of genital herpes was 131.9 per 100, 000 (424 cases) which significantly higher than England’s rate, which is less than half of Wandsworth’s (58.1). in 2013, the rate was similar: 137.0 per 100,000 (429 cases), and the overall trend shows no significant change and has remained consistently worse than England.
4.2.5 Anogenital Warts
Genital warts are causes by strains of the HPV virus and can be very uncomfortable but can easily be treated. HPV vaccine (Gardasil) protects against four strains of HPV that can cause cancer, and prevents genital warts.
Wandsworth had the highest rate of anogenital warts in England in 2016 with a rate of 249.2 per 100,000 (785 cases) and is double England’s rate (112.4). However, it is slightly lower than the 2013 rate (263. 5 per 100, 000 with 825 cases). The overall trend shows no significant change and has remained consistently higher than England.
Figure 1: Number of cases of Anogenital warts (first episode) diagnosed in residents in Wandsworth 2012 – 2016
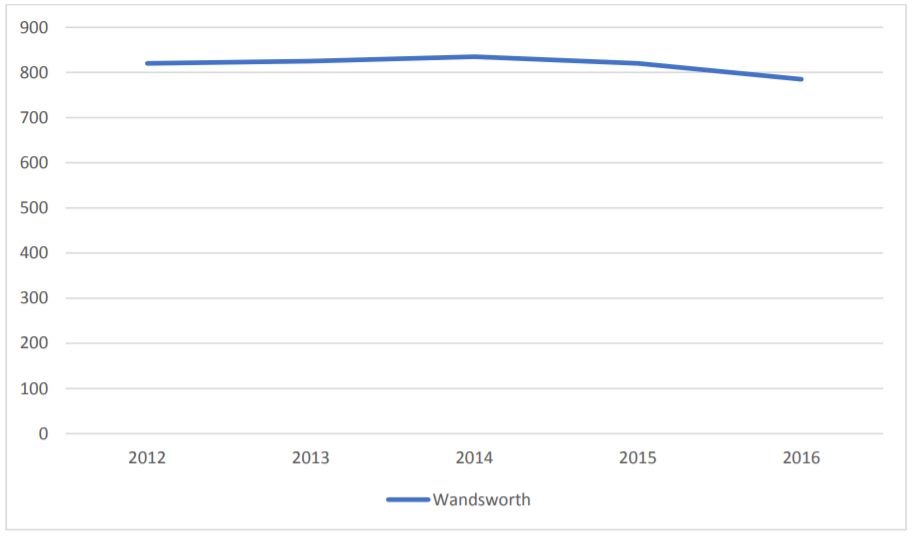
Source: Data from routine specialist and non-specialist sexual health services’ returns to the GUMCAD STI Surveillance System. Excludes chlamydia data from routine non-specialist sexual health services’ returns to the CTAD Chlamydia Surveillance system (CTAD). Rates based on the 2011 ONS population estimates.
4.2.5.1 HPV Vaccination
HPV vaccine (Gardasil) protects against four strains of HPV that can cause cancer and prevents genital warts. It is routinely offered to girls aged 12 to 13 years, and more recently to MSM, trans men and trans women who are eligible, helps to protect against genital warts and cervical cancer. In 2016 81.4% of 12 -13-year-old girls in Wandsworth received the HPV vaccine in 2016, which is similar to London and England
The vaccination prevents at least 70% of cancers of the cervix and potentially more in the future. As it usually takes between 10 and 20 years for a cancer to develop after HPV infection the reduction in the number of cases of pre-cancerous changes in the cervix will only be seen in the longer term.
4.3 HIV
HIV is a life-long condition, which currently has no cure but with early diagnosis and treatment people can maintain their everyday life. Early diagnosis and treatment can also limit transmission.
Nationally, there has been a decline in HIV diagnosis in MSM for the first time in over 30 years as well as continued decline in black heterosexual men and women. However, rates amongst white heterosexual men and women have remained at a similar level for the last 10 years (PHE, 2017)
Wandsworth is classed as a high prevalence area. NICE guidance classifies between 2 and 5 cases of diagnosed HIV per 1,000 people aged 15-59 years as high prevalence. This compares with 2.3 per 1000 nationally. Universal testing is recommended for high prevalence areas.
The rate of new diagnosis is higher than in England. In 2016, 71 residents aged 15 years and above were newly diagnosed with a rate of new HIV diagnosis per 27.2 100,000 population compared to 10.3 in England. HIV testing coverage among SHS patients is higher in Wandsworth than England (77% compared with 67.7%).
The diagnosed HIV prevalence rate is almost double that of England at 5.5 per 1,000 population aged 15-59 years (compared to 2.3 per 1,000 in England). However, in Wandsworth, between 2014 and 2016, almost a third (32%) of people diagnosed with HIV were diagnosed late, compared with 40.1% in England. Late diagnosis can result in damage to the immune system and transmission to others. Of those diagnosed late, 21.9% of men who have sex with men (MSM) and two-thirds (66.7%) of heterosexuals.
In 2016, 1380 residents in Wandsworth received HIV-related care: 1100 males and 285 females. This represents a 15.4% change from 2012 to 2016. Among these, 58.0% were white, 21.0% black African and 6.2% black Caribbean. With regards to exposure, 63.8% probably acquired their infection through sex between men and 30.1% through sex between men and women (PHE, 2017).
In 2016, an estimated 89,400 people were living with HIV infection in England, of whom an estimated 10,400 (approximately 11.6%) were unaware and at risk of unknowingly passing on the virus to sexual partners. If this is applied to the Wandsworth population, it would equate to about 181 people.
4.4 Health Inequalities
In Wandsworth, like England, young heterosexual adults, black ethnic minorities and MSM experience poor sexual health disproportionately.
4.4.1 Age
Young People
Young people aged 15-24 years of age made up almost a third (32%) of new STI diagnosis in 2016. This is significantly less than England where over half (51%) of diagnoses were in this age group. (PHE, 2017).
However, Wandsworth has the 10th highest rate (out of 326 local authorities in England) of new STIs excluding chlamydia diagnoses in 15-24-year olds; with a rate of 1,991.9 per 100,000 residents (compared to 795 per 100,000 in England). Young people disproportionately experience the burden of sexual health as the largest population group is 25-44-year olds; nearly half of all people living in Wandsworth are in this age group. It has the highest proportion of people aged 30-34 years creating a young population ‘bulge’ which is unique nationally (JSNA, 2018).
Older adults
Over the last 60 years’ sexual lifestyles in Britain have changed significantly especially amongst women. Sexual activity continues into later life, so a life course approach is needed (Mercer et al, 2013)
With more older people than in previous generations becoming newly single through divorce, separation, or the death of their partners. Many older people may have incomplete or incorrect knowledge about sexual health and therefore don’t use condoms to reduce the risk of contracting STIs when beginning new sexual relationships.
In 2016, 7% (396) of new STIs were diagnosed in Richmond residents aged between 45
and 65 years of age.
4.4.2 Lesbian, gay, bisexual, trans gender, questioning and intersex people
In 2016, 41.4% (1345) of new STI diagnosis in Wandsworth resdients were among gay, bisexual and other men who have sex with men (MSM), which is an increase from 37.6% (1152 diagnoses) in 2013. ONS estimates suggest 2.6% (6,000) of Wandsworth residents identify as lesbian, gay, bisexual(ONS, 2018). When applied to new STI diagnoses this represents 22% of the LGB population being diagnosed with a new STI, which is significantly higher than the general population.
The number of STI diagnoses in MSM has risen sharply in England over the past decade. This is possibly due to:
- Condomless sex associated with HIV seroadaptive behaviours or sexual behaviours employed by homosexual men to reduce the risk of transmitting or acquiring HIV while engaging in unprotected anal intercourse (UAI). For HIV negative men, these are serosorting (restricting any UAI to sexual partners who are also HIV-negative), and strategic positioning (restricting UAI to taking the insertive role only).
- ‘Chemsex’ (the use of drugs before or during planned sexual activity to sustain, enhance, disinhibit or facilitate the experience).
- Increased screening of MSM has improved detection of gonococcal and chlamydial infections, but has had less impact in recent years as it has become more established. (PHE, 2017)
Gonorrhoea diagnosis in MSM in England decreased between 2015 and 2016, following year on year rises since 2008. This coincides with reductions in HIV diagnoses which are associated with improved HIV testing uptake at STI clinics, including repeat testing. When combined with increased STI testing uptake at STI clinics, this has potentially facilitated prompt identification and treatment of asymptomatic infection which reduces the likelihood of secondary transmission. However, gonorrhoea remains the most commonly diagnosed STI amongst MSM.
Research shows that nationally teenage lesbian or bi-sexual women are at increased risk of unintended pregnancy compared to their peers. Although there is a lower rate of pregnancy in LBWSW than the general population (around half of LBWSW are parents), there is a statistically significant higher rate of pregnancy in adolescent lesbians and bisexual women. In bisexual adolescents the rate was twice that of a heterosexual adolescent. This may be due to the higher reported rates of forced sex* amongst LBWSW compared with the general population (Hodson, Meads and Bewley. 2017).
4.4.3 Ethnicity
Black people, especially those from black African ethnic groups, are more at risk of sexually transmitted infections, including HIV. Black and minority ethnic (BME) groups make up 29% of the overall population (or over 90,000 residents) and account for more than half the population of Tooting (52.7%) (JSNA, 2018). However, the STI rate is higher in the black population than the white population (2366 per 100,000 v 1569 per 100,000) despite two/thirds(67.6%) of diagnosis in white population and less a fifth (15.2%) in black population.
4.4.4 Deprivation
Nationally deprivation and socio-economic status are associated with poorer sexual health and higher teenage (PHE, 2018, Tanton et al., 2015). The chart below shows a clear association in Wandsworth between poor sexual health and deprivation with those in quintile 5 (the most deprived) experiencing the poorest sexual health.
* Forced sex is a type of sexual abuse, defined by ChildLine as ‘being forced to have sex (intercourse), look at sexual pictures or videos, do something sexual” and it can also refer to being pressured to engage in sexual activity in return for money or drugs, often referred to as ‘transactional sex’.
Figure 2: Rates* per 100,000 population of new STIs by deprivation category in Wandsworth (SHS diagnoses only): 2016
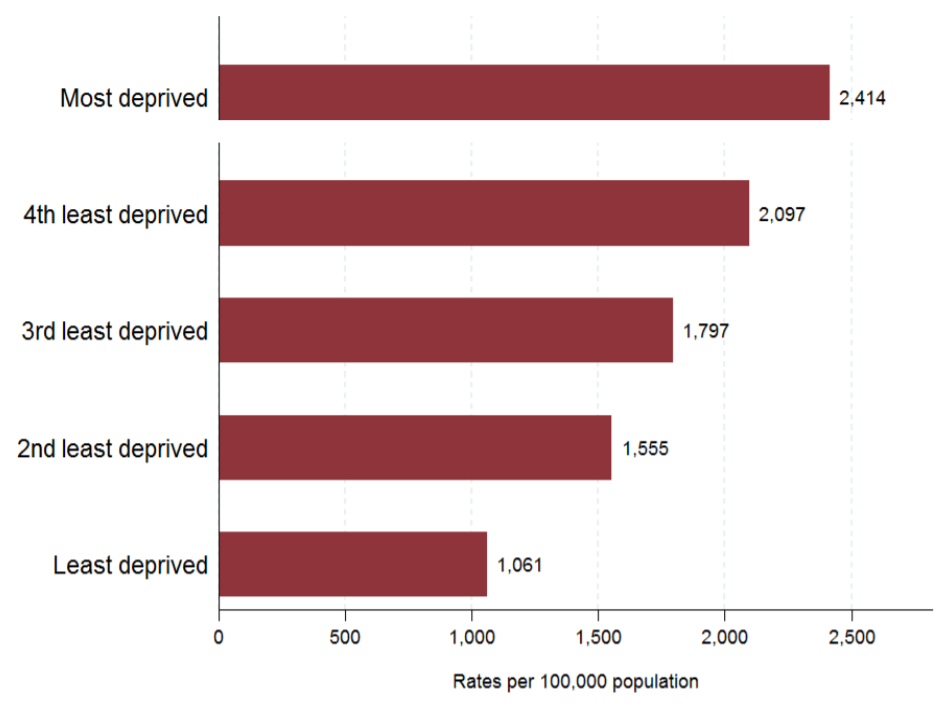
Source: Data from routine specialist and non-specialist sexual health services’ returns to the GUMCAD STI Surveillance System. Excludes chlamydia data from routine non-specialist sexual health services’ returns to the CTAD Chlamydia Surveillance system (CTAD). Rates based on the 2011 ONS population estimates. Deprivation quintiles generated from Index of Multiple Deprivation (IMD) scores 2011. Excludes chlamydia diagnoses made outside SHS.
*Lower Layer Super Output Areas (LSOA) are built from groups of contiguous Output Areas and have been automatically generated to be as consistent in population size as possible, and typically contain from four to six Output Areas. The minimum population is 1,000 and the mean is 1,500. (Laser Report, 2017)
4.4.5 People with disabilities
People with a disability have the same sexual health needs as other people. However, they are much less likely to have access to information on sexual health because of attitudes towards disability and sexuality, lack of resources and lack of professionals qualified to provide the right kind of information and appropriate support. It is estimated that 10% (approximately 31,454) of Wandsworth residents have a disability affecting their day to day life (JSNA, 2018).
4.4.6 Homeless People
Homeless people are at greater risk of poor sexual health compared with the general population. This includes STIs and unplanned pregnancies and they may be vulnerable to sexual abuse; for example, if they come under pressure to exchange sex for food, shelter, drugs and money.
The rate of family homelessness in Wandsworth has increased year on year from 4.7 per 1,000 households in 2011/12 to 6.3 per 1,000 in 2015/16. In common with most London authorities, homelessness is significantly higher than the England average of 2.5 per 1,000 households (JSNA, 2018). The number of rough sleepers in Wandsworth is relatively low compared to other inner London boroughs, although it has increased from 62 in 2011/12 to 96 in 2015/16 (JSNA, 2018).
4.4.7 Sex Workers
There is limited data available about sex workers. However, female sex workers are assumed to be at increased risk of sexually transmitted infections (STIs) but there are limited comparative data with other population groups available.
Estimates suggest 60 000-80 000 sex workers live in the UK and approximately 80% are women, who work on the streets or in various indoor environments (HOC, 2016). However, most sex workers are now thought to operate online. 9% of British men have admitted previously paying for sex.
4.4.8 Sexual Health Knowledge amongst Young People
Research undertaken by Participation People showed that young people want more information on sexual health, issues and SRE topics. They had a poor understanding of STIs, misinformation about consent and acceptable sexual behaviour and negative attitudes towards condoms as they believed in reduced pleasure. The research also showed that social media has a huge influence on young people’s views and attitudes.
From September 2020, state primary and secondary schools will have a statutory duty to deliver RSE (Relationships and Sex Education). Currently sex and relationship education (SRE) is delivered by teachers, school nursing service, voluntary agencies and youth service.
4.4.9 Child Sexual Exploitation
Child sexual exploitation (CSE) is a type of sexual abuse in which children are sexually exploited for money, power or status. A common feature of CSE is that the child or young person does not recognise the coercive nature of the relationship and does not see themselves as a victim of exploitation.
The complex and hidden nature of Child Sexual Exploitation means that it is very difficult to provide an accurate number of either current or former victims.
4.4.10 Risky Behaviour
The cumulative risk from multiple unhealthy behaviours is significant and these risk-taking behaviours can also play a role in influencing risky sexual behaviour. It is estimated that 12% of 15-year-olds in Wandsworth partake in 3 or more risky behaviours (including smoking, drinking, and cannabis, use of other drugs, poor diet and low physical activity). This is similar to the London average (10%) and lower than the England average (16%) (What About YOUth? Survey 2014/15).
Risky behaviour is also associated with sexting, sexual health and mental health and Chemsex.
5. Local Services
National Context
Sexual health services are commissioned at a local population level to meet the needs of the local population. These services provide information, advice and support on a range of issues, such as sexually transmitted infections (STIs), contraception, relationships and unplanned pregnancy.
Local authorities have a statutory duty to commission comprehensive open access sexual health services (including free STI testing and treatment, notification of sexual partners of infected persons and free provision of contraception) for their residents. However, some specialised services are directly commissioned by clinical commissioning groups (CCGs), and at the national level by NHS England.
Local Context
The London Borough of Wandsworth (LBW) commissions CLCH to provide a comprehensive open access sexual health service. The service is jointly commissioned with the London Boroughs of Merton and Wandsworth.
LBW also commissions sexual health services including Chlamydia screening and treatment, partner notification and Emergency Hormonal Contraception (EHC) via primary care. Additional preventive services are provided by the voluntary sector and through schools, school nursing and the youth service.
Sexual health services currently focus on treatment for sexual health transmitted infections, HIV and unplanned pregnancies as well as prevention. Evidence shows that increased preventive work has the potential to deliver savings not only to sexual health commissioners but to the whole system.
5.1 Integrated Sexual Health Service
The integrated model provides screening and treatment for STIs as well as contraception. There are currently two hubs and several spokes, but a larger hub near Clapham Junction Stations will replace the smaller hubs in October 2018. Hubs provide the full range of sexual health services (levels 1-3)† and spokes provide services (levels 1-2)‡
Data from Pathway Analytics for October 1st, 2017 -31st March 2018 shows that attendances amongst 18-24-year-old population have decreased since that the new service commenced by 16% compared with attendances at the previously commissioned services the same time period in the year.
Since the introduction of the new service the percentage of attendances by residents at Wandsworth services has increased but the percentage of residents accessing services outside the borough has also increased; more than half of residents now access services outside the borough.
Between 1st October 2017- 31st March 2018 63% of attendances at sexual health services in Wandsworth were Wandsworth residents. 39% attended a service based in Wandsworth. 27.2% of Wandsworth residents attended Balham Health Centre, 12.4% attended Dean Street Clinic, 11.4% attended Queen Mary’s Hospital and 10% attended the John Hunter Clinic.
This compares to between 1st October 2016- 31st March 2017 when 55.8% of attendances at sexual health services in Wandsworth were Wandsworth residents. Half (51%) of residents attended a service based in Wandsworth. Almost a third (32.9%) of Wandsworth residents attended St George’s Hospital, 13.3% of residents attended Dean Street Clinic and 9.6% of residents attended Queen Mary’s Hospital.
† See Appendix 1 for a definition of service provision by level.
‡ See Appendix 1 for a definition of service provision by level.
5.2 General Practice
5.2.1 LARC
In general practice between 2015-18, 1,124 IUDS were fitted and 592 removed, 2,767 were fitted and 1,243 removed, and 1,208 implants were inserted and 1,109 removed.
5.3 Community Pharmacy
Community pharmacies are commissioned to deliver level 1 and 2 sexual health services. This includes Emergency Hormonal Contraception (EHC) for women over the age of 16, Chlamydia screening for 16-24 years of age and free condoms via the Come Correct condom distribution scheme.
5.3.1 Chlamydia Screening
In General Practice in 2016-17 there were 2,962 screens in general practice with 28 positives and 163 screens in community pharmacy with 13 positives.
5.3.2 Emergency Hormonal Contraception
Between 2015-2018, 10,848 EHC were prescribed in community pharmacies.
5.4 Condom Distribution
The Come Correct (or CCard) scheme provides access to free condoms in a variety of locations (called Outlets) across London. Once registered, young people can collect condoms for free or get advice from any Outlet displaying the Come Correct logo. In Wandsworth the scheme is administered by Metro.
Between October 2017 and April 2018, 101 young people registered for the scheme in the borough. All the young people accessing the service were Wandsworth residents.
6. Conclusion
Overall the sexual health of the Wandsworth population is significantly worse when compared to London and England. The burden of sexual ill health is disproportionate across the population; young people, black ethnic groups and men who have sex with men are more likely to suffer sexual ill health. Young people and MSM are the largest groups diagnosed with a new STI and, although the teenage pregnancy rate is similar to England and London, there are other boroughs with rates that are half that of Wandsworth. The black population experience a significantly higher proportion of STI diagnoses compared with the proportion of the population from this ethnic groups. STI diagnosis is increasing amongst men who have sex with men. Since the introduction of the new ISH service the proportion of residents attended sexual services in Wandsworth has decreased, particularly amongst young people aged between 18-24 years old.
7. Recommendations
Six priorities for action have been identified:
- To reduce the prevalence of sexually transmitted infections
- To reduce unplanned pregnancies
- To continue to reduce teenage pregnancy
- To reduce late HIV diagnosis
- To reduce risky behaviour and improve sexual health
- To take a whole systems approach to addressing priorities 1-5
8. References
FPA. (2015) Unprotected Nation 2015: An update on the Financial and Economic
Impacts of Restricted Contraceptive and Sexual Health Services. 2015.
Hodson, Meads and Bewley. (2017) Hodson, K., Meads, C. and Bewley, S. (2017) Lesbian and bisexual women’s likelihood of becoming pregnant: a systematic review and metaanalysis. BJOG: An International Journal of Obstetrics and Gynaecology, 124 (3). pp. 393- 402
House of Commons (HOC), (2016) House of Commons Home Affairs Committee
Prostitution Third Report of Session 2016-17
London Borough of Wandsworth (2018) Joint Strategic Needs Assessment (JSNA)
Lee, E., Clements,S., Ingham, R. and Stone, N. (2004) A matter of choice? Explaining national variation in teenage abortion and motherhood Rowntree Foundation: York
Mercer C. H. Et al (2013) Changes in sexual attitudes and lifestyles in Britain through the life course and over time: findings from the National Surveys of Sexual Attitudes and Lifestyles (Natsal) The Lancet 382(9907); 1781 – 1794
Montouchet C, Trussell J. (2013) Unintended pregnancies in England in 2010: costs to the National Health Service (NHS). Contraception. 2013;87(2):149-53.
ONS (2018) ww.ons.gov.uk [accessed 19th September 2018]
Public Health England (PHE) (2017) Local Authority STI and HIV Epidemiology Report (LASER): London Borough of Wandsworth PHE: London
Public Health England (PHE) (2017) Local Authority STI and HIV Epidemiology Report (LASER): London Borough of Wandsworth PHE: London
Public Health England (PHE) (2018) National Teenage Pregnancy Prevention Framework PHE: London
World Health Organisation (WHO) www.who.org [accessed 3rd September 2018]
Appendix 1
Sexual Health Service Definition of Levels
Level 1
- Sexual history-taking and risk assessment: Including assessment of need for emergency CONTRACEPTION and Human Immunodeficiency Virus (HIV) postexposure prophylaxis following sexual exposure (PEPSE)
- Signposting to appropriate Sexual Health Services
- Chlamydia screening: Opportunistic screening for genital chlamydia in asymptomatic males and females under the age of 25
- Asymptomatic Sexually Transmitted Infection screening and treatment of asymptomatic infections (except treatment for syphilis) in men (excluding men who have sex with men) and women
- Partner notification of Sexually Transmitted Infections or onward referral for partner notification
- Human Immunodeficiency Virus testing: Including appropriate pre-test discussion and giving results
- Point of care Human Immunodeficiency Virus testing: Rapid result Human Immunodeficiency Virus testing using a validated test (with confirmation of positive results or referral for confirmation)
- Screening and vaccination for Hepatitis B: Appropriate screening and vaccination for Hepatitis B in at-risk groups
- Sexual health promotion: Provision of verbal and written sexual health promotion information
- Condom distribution: Provision of condoms for safer sex
- Psychosexual problems: Assessment and referral for psychosexual problems
Level 2
Level 2 Sexual Health Services incorporate Sexual Health Services provided by a Level 1
Sexual Health Service plus:
- Intrauterine Device/System (IUD/IUS) insertion and removal (including emergency IUD)
- CONTRACEPTION implant insertion and removal
- Counselling and referral for vasectomy
- Sexually Transmitted Infection (STI) testing and treatment of symptomatic but uncomplicated infections in men (except men who have sex with men) and women excluding: men with dysuria and/or genital discharge, symptoms at extra-genital sites, e.g. rectal or pharyngeal, pregnant women, genital ulceration other than uncomplicated genital herpes.
Commissioned Level 2 Sexual Health Services include:
- Enhanced General Practices
- Sexual and Reproductive Health Services
- Integrated services (joint Genitourinary Medicine and Sexual and Reproductive Health
Services) - Young people clinics such as Brook
- Other NHS commissioned Sexual Health Services Level 3
Level 3
Level 3 Genitourinary Medicine Services provide Sexually Transmitted Infection (STI) management and include SERVICES provided by Level 1 Sexual Health Services and Level 2 Sexual Health Services plus:
- Sexually Transmitted Infection testing and treatment of men who have sex with men
- Sexually Transmitted Infection testing and treatment of men with dysuria and genital discharge
- Testing and treatment of Sexually Transmitted Infections at extra-genital sites
- Sexually Transmitted Infections with complications, with or without symptoms
- Sexually Transmitted Infections in pregnant women
- Recurrent or recalcitrant Sexually Transmitted Infections and related conditions
- Management of syphilis at all stages of infection and blood borne viruses
- Tropical Sexually Transmitted Infections
- Specialist Sexually Transmitted Infection (HIV) treatment and care
- Provision and follow up of Sexually Transmitted Infection post exposure prophylaxis
(PEP), both sexual and occupational - Sexually Transmitted Infection service co-ordination across a network including:
- Clinical leadership of Sexually Transmitted Infection management
- Co-ordination of clinical governance
- Co-ordination of Sexually Transmitted Infection training
- Co-ordination of partner notification
Glossary
BME Black and minority ethnic
CCG Clinical Commissioning Group
DoH Department of Health
EINA Equality Impact Needs Assessment
EHC Emergency hormonal contraception
GPs General Practitioners
HIV Human immunodeficiency virus
LARC Long acting reversible contraception
LGBTQI Lesbian, gay, bisexual, transgender, questioning and intersex
LSHTP London Sexual Health Transformation Programme
MSM Men who have sex with men
NHS National Health Service
NHSE National Health Service England
NICE National Institute for Health and Care Excellence
PHE Public Health England
PrEP Pre-Exposure Prophylactic
RSE Relationships and sex education (the new name for SRE)
SRE Sex and relationship education
STIs Sexually Transmitted Infections
UDM User dependent methods
WHO World Health Organisation
WSW Women who have sex with women
Document Information
Published: 2018
For Review: 2022
Public Health Topic Lead: Hannah Gill, Public Health Lead
